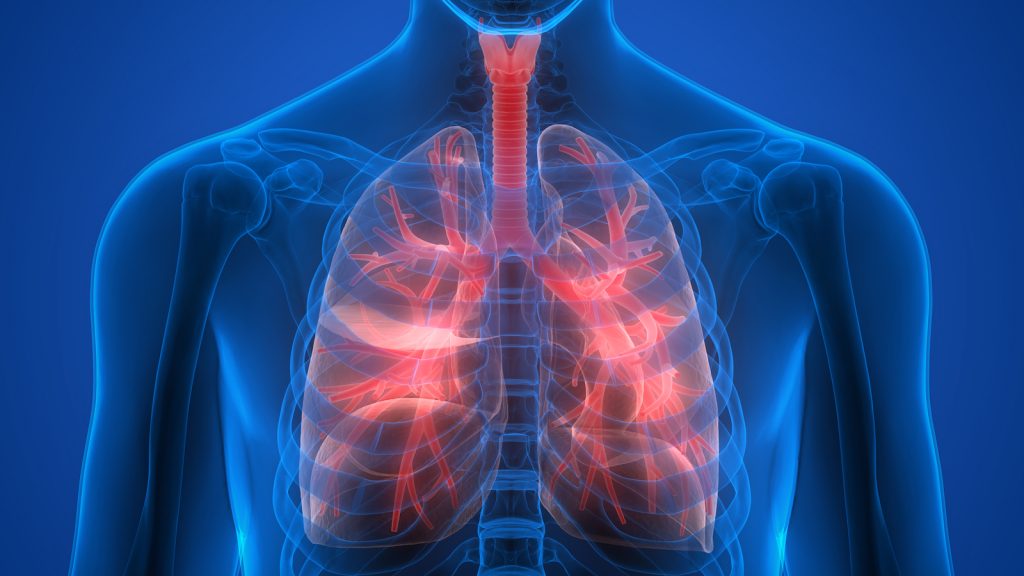
Variations in lung anatomy alone may explain why an individual is more likely than another to develop chronic obstructive pulmonary disease (COPD). This is the conclusion of a team of researchers from the Research Institute of the McGill University Health Center (RI-MUHC) and Columbia University. The researchers examined CT scans of more than 3,000 patients with and without COPD, a progressive lung disease that causes inflammation of the airways, making breathing difficult. About sixteen percent of people have an excess airway section in the lungs, and six percent have a missing section, while four percent display a combination of variants or a different configuration. The results of the study were published online January 16, in Proceedings of the National Academy of Sciences.
COPD is characterised by inflammation of the bronchi and remodelling of the bronchi. It causes progressive obstruction of the airways and difficulty breathing. Of exacerbations, i.e. a sudden worsening of symptoms, occurring in 80% of patients and often leads to hospitalisation and an excess risk of death in the months and years following – this is the problem the researchers wanted to target.
In two other respiratory diseases, asthma and fibrosis In the lungs, there is an increase in the concentration of fibrocytes, bone marrow stem cells that pass into the blood and colonise the inflamed regions, contributing to the aggravation of these diseases. In the case of asthma, these cells differentiate into smooth muscle cells (myocytes) that increase the contractions of the bronchi. In case of pulmonary fibrosis, fibrocytes differentiate into fibroblasts (tissue support cells) and accentuate fibrosis.
Forest Medical Spirometer Calibration
Spirometry is a breathing or ‘lung function’ test. It’s one of the most common tests people with asthma, or people who are being tested for asthma, are given. Your GP or asthma nurse will ask you to take a deep breath and then breathe out as fast as you can and for as long as you can through a mouthpiece linked to a ‘Spirometer’. You will have to blow a few times so your GP or asthma nurse can get an accurate result.
As with all medical equipment, Spirometers need thorough and comprehensive testing on a regular basis. Failure to adequately test a Spirometer puts it at risk of failure or of false readings being displayed from the equipment, which can have disastrous results.
We undertake thorough Spirometer Calibration to fully test your machines and ensure that they are safe and suitable for use.